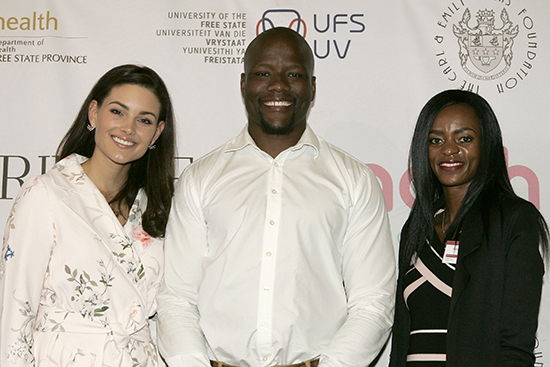
Rolene Strauss Patron of the MACAH Foundation, Oupa Mohoje,
Cheetahs rugby union player, and Kesa Molotsane
who are both champions of the MACAH Foundation.
Photo: Johan Roux

From left is: Prof Gert van Zyl, MACAH Foundation’s founding
Director and Chairman; Khumo Selebano,
newly appointed Director; Dr Riana van Zyl founding director,
and Prof Andre Venter, Founding director and Project Leader.
Photo: Johan Roux
The Mother and Child Academic Hospital (Macah) Foundation was launched at the University of the Free State (UFS) on 24 April 2018. The foundation is instrumental in the building of a state-of-the-art academic hospital that will provide antenatal care and comprehensive health services for mothers, infants and children in Central South Africa. The hospital will be developed under a project in a partnership between UFS, Afrisky Holdings, and the Free State Department of Health, and will be located on the university’s Bloemfontein Campus but will be privately owned and operated.
Prof Francis Petersen, UFS Rector and Vice-Chancellor, said in his opening remarks this high-level partnership was a demonstration of the power of working together to implement innovation and development, promoting research and academic excellence, while serving communities that are most in need. “This project is possibly the first of its kind in South Africa. I am really proud that the UFS can be a part of it,” he said.
Officials from the Mangaung Metropolitan Municipality; Deputy Director General of the Free State Department of Health, Mr Sekgothe Polelo; members of the UFS rectorate; senior academics in the Faculty of Health Sciences; Dr Rolene Strauss, former Miss World and patron of the Macah Foundation; as well Kesa Molotsane, athlete and UFS student, who is the new face of the Macah Foundation, as well as Oupa Mohoje, Springbok rugby player and captain of the Toyota Free State Cheetahs, who is also the face Macah Foundation among others, were present at the event. Prof Gert van Zyl, Dean of the Faculty of Health Sciences, said the university had a pivotal role to play in shaping the future of children who are the future generation. “If we fail our children, we fail our future, our culture and our being,” he said.
The Macah Foundation’s “Make the first 1000 Days Count” programme emphasises the importance of childcare in the first 1000 days. By the age of five, almost 90% of a child’s brain will be developed. Therefore, it is vital that this period is well monitored to ensure the child grows to be a vigorous and happy individual. As nurturer, a mother’s health is just as significant from conception to birth and beyond. The R20-million programme is still in its early stages, but has already received great support.
Prof André Venter, one of the founding directors of Macah, and Head of Paediatrics and Child Health at the UFS Faculty of Health Sciences, said the success of the mother and child hospital was like a dream come true.
“We have been working on this concept for seven years. It is a privilege for me to work with children, but more so when we can combine so many skills and expertise in developing a world-class facility that will help members of our communities to thrive.”
The foundation is growing steadily and its founding directors are calling on corporates, businesses, and individuals to support it through their influence, loyalty and financial means.
To find out more about the foundation and pledge your support, visit www.macahfoundation.org.za or send an email to Tertia de Bruin on debruintr@ufs.ac.za or foundation@macahfoundation.org.za