 |
|
Ph.D students, Chantel Swart and Ntsoaki Leeuw
|
Scientists at the University of the Free State (UFS) made an important breakthrough in the use of nanotechnology in medical and biological research. The UFS team’s research has been accepted for publication by the internationally accredited Canadian Journal of Microbiology.
The UFS study dissected yeast cells exposed to over-used cooking oil by peeling microscopically thin layers off the yeast cells through the use of nanotechnology.
The yeast cells were enlarged thousands of times to study what was going on inside the cells, whilst at the same time establishing the chemical elements the cells are composed of. This was done by making microscopically small surgical incisions into the cell walls.
This groundbreaking research opens up a host of new uses for nanotechnology, as it was the first study ever in which biological cells were surgically manipulated and at the same time elemental analysis performed through nanotechnology. According to Prof. Lodewyk Kock, head of the Division Lipid Biotechnology at the UFS, the study has far reaching implications for biological and medical research.
The research was the result of collaboration between the Department of Microbial, Biochemical and Food Biotechnology, the Department of Physics (under the leadership of Prof. Hendrik Swart) and the Centre for Microscopy (under the leadership of Prof.Pieter van Wyk).
Two Ph.D. students, Chantel Swart and Ntsoaki Leeuw, overseen by professors Kock and Van Wyk, managed to successfully prepare yeast that was exposed to over-used cooking oil (used for deep frying of food) for this first ever method of nanotechnological research.
According to Prof. Kock, a single yeast cell is approximately 5 micrometres long. “A micrometre is one millionth of a metre – in laymen’s terms, even less than the diameter of a single hair – and completely invisible to the human eye.”
Through the use of nanotechnology, the chemical composition of the surface of the yeast cells could be established by making a surgical incision into the surface. The cells could be peeled off in layers of approximately three (3) nanometres at a time to establish the effect of the oil on the yeast cell’s composition. A nanometre is one thousandth of a micrometre.
Each cell was enlarged by between 40 000 and 50 000 times. This was done by using the Department of Physics’ PHI700 Scanning Auger Nanoprobe linked to a Scanning Electron Microscope and Argon-etching. Under the guidance of Prof. Swart, Mss. Swart en Leeuw could dissect the surfaces of yeast cells exposed to over-used cooking oil.
The study noted wart like outgrowths - some only a few nanometres in diameter – on the cell surfaces. Research concluded that these outgrowths were caused by the oil. The exposure to the oil also drastically hampered the growth of the yeast cells. (See figure 1)
Researchers worldwide have warned about the over-usage of cooking oil for deep frying of food, as it can be linked to the cause of diseases like cancer. The over-usage of cooking oil in the preparation of food is therefore strictly regulated by laws worldwide.
The UFS-research doesn’t only show that over-used cooking oil is harmful to micro-organisms like yeast, but also suggests how nanotechnology can be used in biological and medical research on, amongst others, cancer cells.
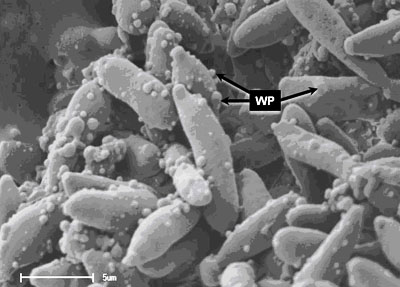
Figure 1. Yeast cells exposed to over-used cooking oil. Wart like protuberances/ outgrowths (WP) is clearly visible on the surfaces of the elongated yeast cells. With the use of nanotechnology, it is possible to peel off the warts – some with a diameter of only a few nanometres – in layers only a few nanometres thick. At the same time, the 3D-structure of the warts as well as its chemical composition can be established.
Media Release
Issued by: Mangaliso Radebe
Assistant Director: Media Liaison
Tel: 051 401 2828
Cell: 078 460 3320
E-mail: radebemt@ufs.ac.za
18 August 2010